Upcoming Endometriosis Awareness Events:
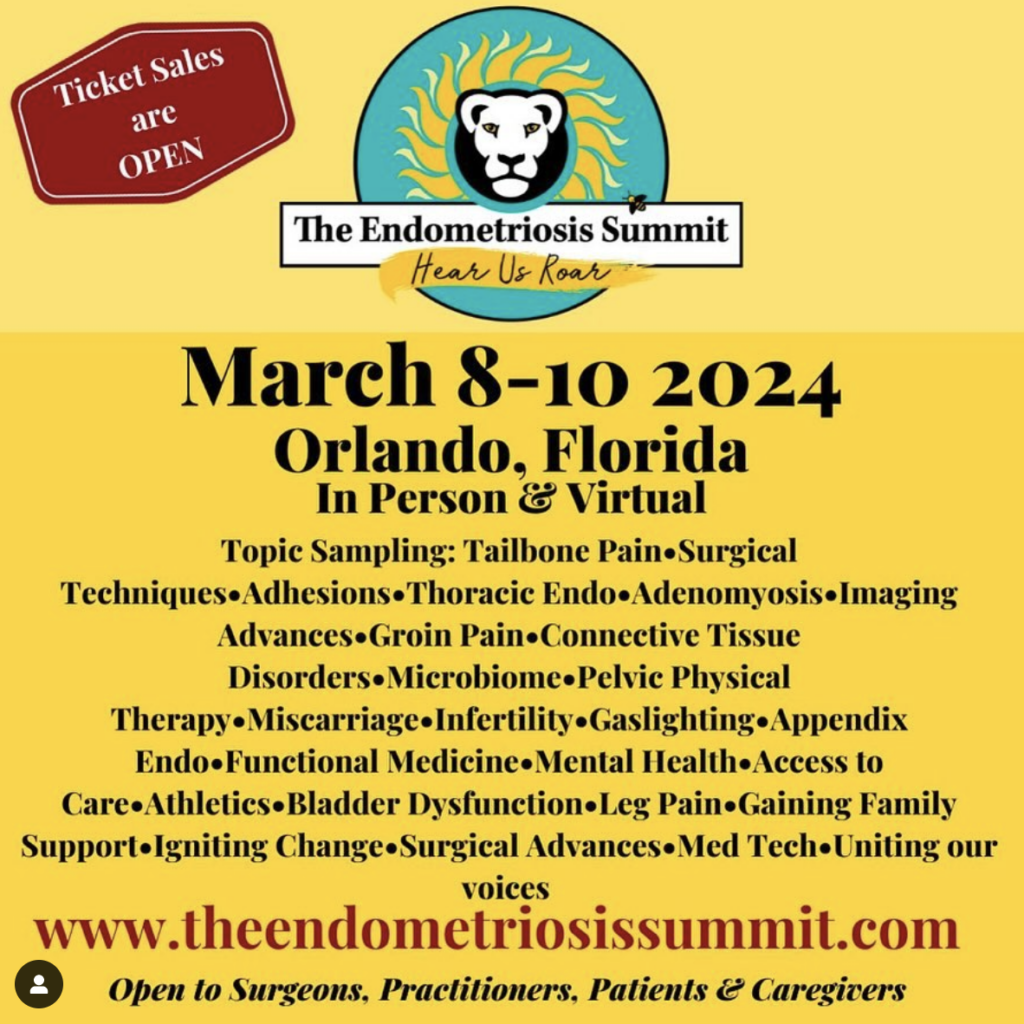
March 8-10, 2024
Endometriosis Summit
https://theendometriosissummit.com/
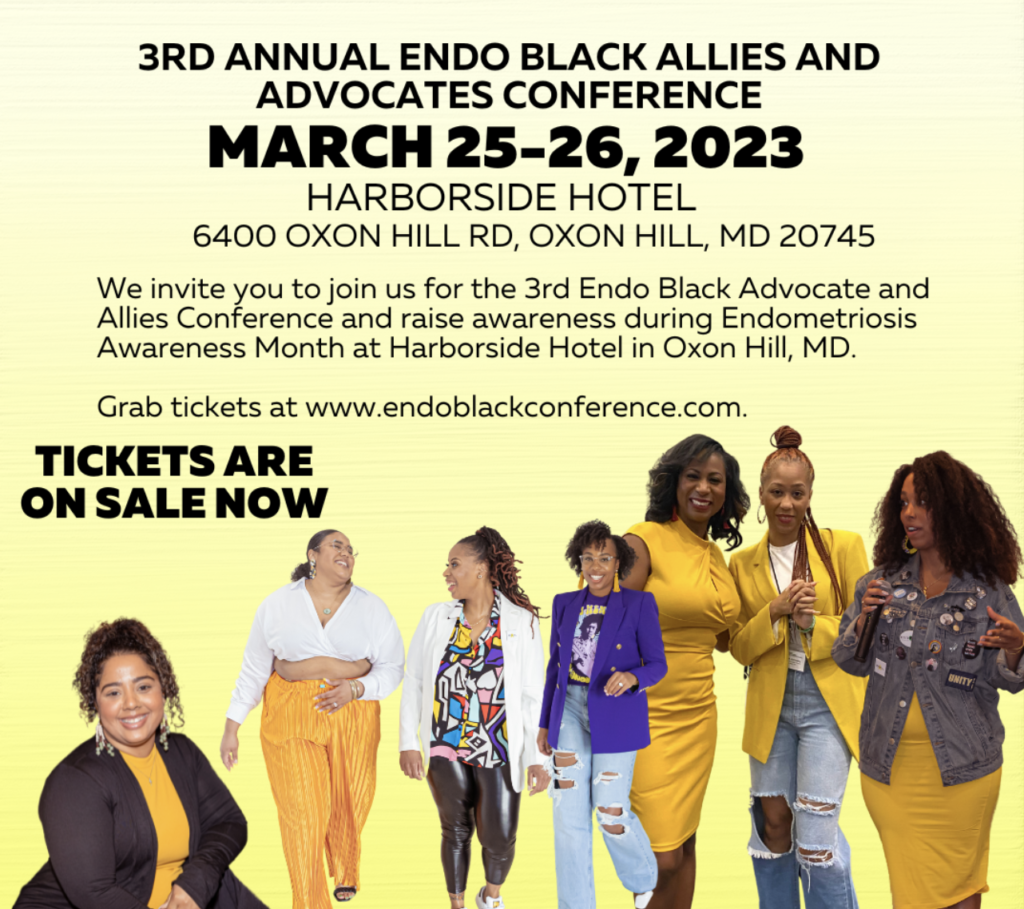
March 16-17, 2024
Endo Black Conference
https://www.endoblack.org/events

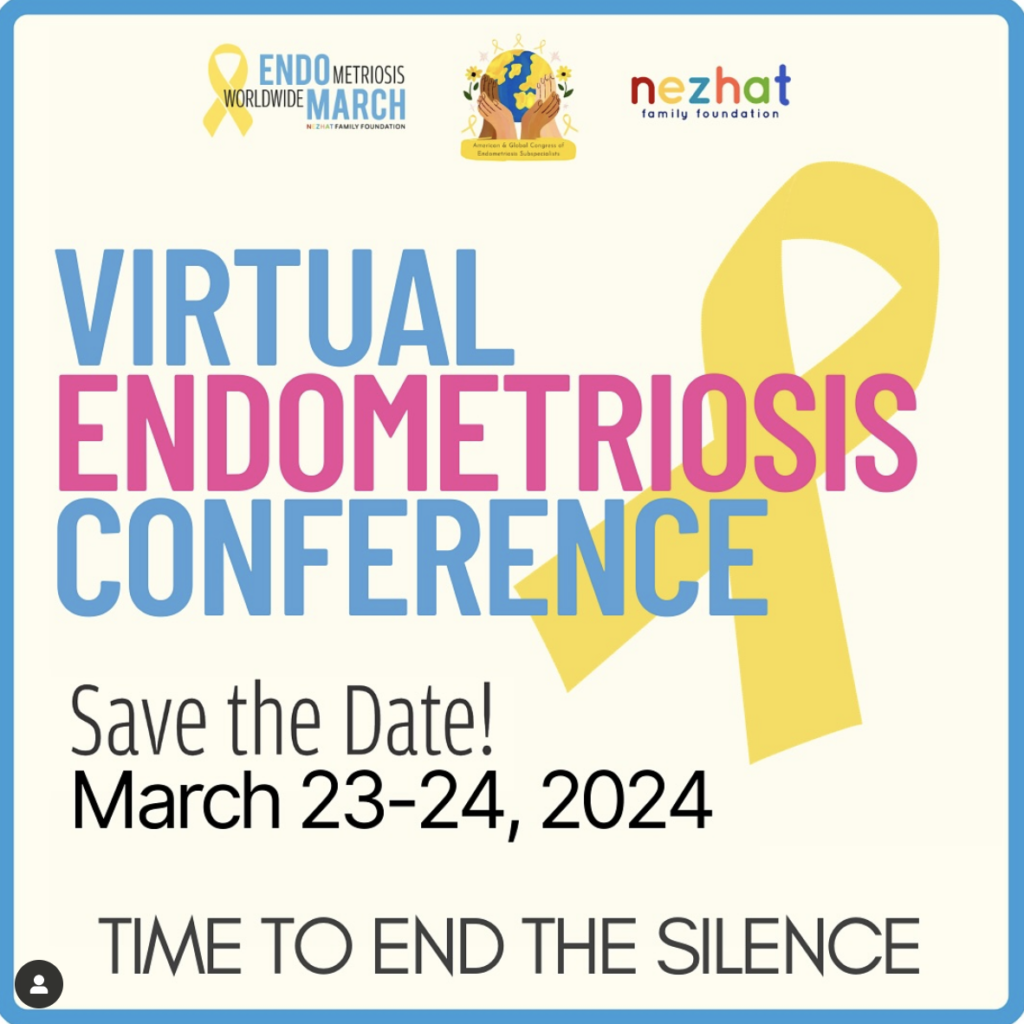
March 23-24, 2024
Virtual Endometriosis Conference
(Worldwide Endo March)
https://nezhat.org/save-the-date-virtual-endometriosis-conference-2024/